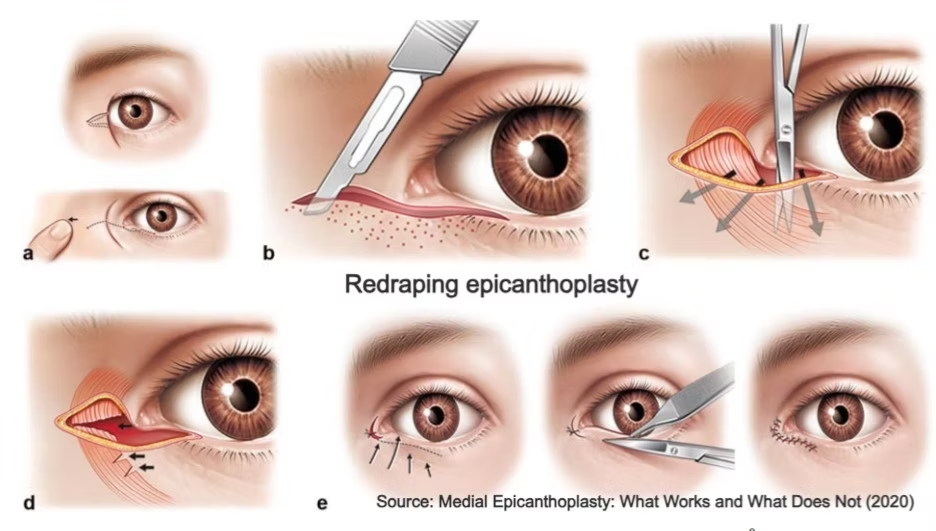
Medial Epicanthoplasty Using Skin Redraping: Enhancing Aesthetic Precision and Scar Concealment
- Jul 23, 2025
- 5 min read
Updated: Sep 8, 2025
In the realm of Asian aesthetic surgery, medial epicanthoplasty remains one of the most frequently requested yet technically sensitive procedures. As detailed by Wong Chin-Ho, MRCS(Ed), FAMS(Plast Surg), and Hsieh Michael Ku Hung, MRCS(Ed), FAMS(Plast Surg) in their 2025 study published in Plastic and Reconstructive Surgery, the epicanthal fold—a fibromuscular web covering the medial canthus and often obscuring the caruncle—is present in up to 90% of Asian patients.
While part of normal anatomy, its prominence may contribute to a “blunted” or closed-eye appearance, prompting many patients to seek surgical correction for a more open, alert, and harmonious gaze. Traditional techniques—such as Z-plasty, V-W flap, and Mustarde’s four-flap epicanthoplasty—focus on skin rearrangement via transposition or excision flaps.
While these methods can effectively reduce the epicanthal fold, they are often associated with visible scarring, particularly in Asian skin types prone to hypertrophic response and pigmentary changes. In recent years, the skin redraping technique has gained popularity across Asia for its refined approach and discreet, scar-concealing outcomes. Rather than relying solely on geometric flap transpositions, this method focuses on releasing the underlying fibromuscular tension and redraping the skin in a tension-free, natural alignment.
Below, we explore the rationale, step-by-step technique, and clinical advantages of this approach.
Understanding the Epicanthal Anatomy

The epicanthal fold is not merely an excess of skin. It is anchored by a fibromuscular core composed of the medial canthal fibrous band (MCFB) and fibers of the preseptal orbicularis oculi. These act like a tethering cable, drawing skin medially to create the characteristic tent over the caruncle.
Effective and lasting correction must therefore involve two critical steps:
Elimination of fibromuscular tension through complete transection of the MCFB and orbicularis fibers.
Conservative skin redraping, tailored to the degree of epicanthal prominence and desired caruncle exposure.
Any technique that fails to fully address this deeper layer risks either under-correction or recurrence. The skin redraping method, in contrast, targets both the superficial and deep causes—delivering long-lasting, natural-looking results with minimal scarring.
Step-By-Step Surgical Technique

The skin redraping medial epicanthoplasty involves both precise dissection and thoughtful skin redraping based on patient-specific anatomy and aesthetic goals. Here’s a breakdown of the technique as performed under loupe or microscope magnification:
1. Surgical Markings
Preoperative design begins by identifying five key landmarks:
Point A: Desired new medial canthus location—adjusted medially or laterally depending on the degree of caruncle exposure desired.
Point B: At the free edge of the epicanthal fold, horizontally aligned with Point A.
Point C: Just medial to the lacrimal lake, typically 4–6 mm from Point A.
Point D: Along the subciliary margin.
Point E: Medially along the supratarsal crease.
These points outline the arc of skin to be undermined and redraped.
2. Anesthesia and IncisionFollowing local anesthesia infiltration:
3. Dissection
The skin is sharply elevated from the orbicularis oculi in a subcutaneous plane extending 3–4 mm laterally from the incisions. The dissection then transitions to the intramuscular plane to raise a composite skin-muscle flap, preserving vascularity and minimizing scarring risk. Medially, dissection stops at Point A, taking care to avoid the lacrimal canaliculus.
Using sharp iridectomy scissors, the MCFB and associated orbicularis fibers are completely transected, releasing the fibromuscular tension that causes the epicanthal fold’s characteristic tenting. This release allows Point A to be approximated tension-free to Point C, effectively correcting the fold at its source.
4. Skin Redraping and Excision
After fibrous release, excess skin is conservatively excised:
A triangular excision superior to Point C is incorporated into the supratarsal fold.
Additional triangular excisions inferior to Point C may be performed as needed.
The key suture is placed between Points A and C using 7-0 Ethilon, ensuring tension-free closure. Remaining incisions are closed carefully in a single layer, aligned with the subciliary margin.
Postoperative Care
Patients are followed closely during recovery. Sutures are removed at day 6, after which scar massage with silicone gel is started. If signs of hypertrophic scarring appear, intralesional injections of triamcinolone (mixed with 5-FU) are initiated at 4 weeks post-op.
In some cases, a microbotulinum toxin injection (1 unit per side) can be beneficial in reducing dynamic muscular tension during healing, particularly in high-risk scarring patients.
Clinical Outcomes & Experience
Long-term follow-up shows consistently natural results with virtually invisible scars, and revision rates below 1%. Even in revision cases, the same technique can be safely reapplied without compromising tissue integrity.
Over 100 patients have undergone this procedure in the past eight years with high satisfaction and low revision rates. Only one patient (0.8%) required a revision, which was successfully completed using the same technique. No cases of visible scarring required correction—testament to the precision and minimal-tension closure strategy.
Why Skin Redraping is Becoming the New Standard
Unlike geometric flap techniques, skin redraping does not merely reshape the skin—it releases the root cause of the epicanthal fold. By eliminating fibromuscular tension and allowing the skin to settle naturally in a tension-free closure, the technique delivers consistently aesthetic results with minimal scarring.
For surgeons working with Asian patients, this approach offers:
Greater customization to patient preferences
Reliable correction across all severities of epicanthal folds
Superior scar concealment, even in high-risk skin types
Easy integration with upper eyelid surgery for optimal results
Since its adoption in 2017, the technique has proven its value in over a hundred cases, with excellent patient satisfaction, no scar revisions, and minimal complications.
Conclusion
Medial epicanthoplasty is no longer a surgery of compromise. Medial epicanthoplasty, when performed using the skin redraping technique, becomes a powerful and elegant tool in the aesthetic surgeon’s repertoire. By combining anatomical precision with minimal scarring and customizable outcomes, this approach addresses both function and form.
Unlike traditional flap-based techniques, it doesn't merely reposition skin—it resolves the tension at its source, enabling natural redraping and restoration of harmony to the medial canthal region.
As more practitioners refine their skills in this method, the future of epicanthoplasty will be defined not by clever flap patterns, but by anatomical precision and aesthetic foresight.
Reference:
Wong, Chin-Ho MRCS(Ed), FAMS(Plast Surg)1; Hsieh, Michael Ku Hung MRCS(Ed), FAMS(Plast Surg)2,3. Medial Epicanthoplasty with the Skin-Redraping Technique: Technical Refinements for Predictable Outcomes. Plastic and Reconstructive Surgery 155(3):p 517e-522e, March 2025. | DOI: 10.1097/PRS.0000000000011533
Learn techniques behind Upper & Lower Blepharoplasty
in our upcoming Master Class:
IFAAS Cadaver Master Class (Hands-On)
Upper & Lower Blepharoplasty Level 1: Suture & Minimally Invasive Techniques
Oct 9, 2025 - Singapore General Hospital - [Register Now]
Oct 10, 2025 - Singapore General Hospital - [Register Now]
Dec 13-14, 2025 - Tokyo, Japan - [Register Now]
Mar 13-14, 2025 - Seoul, South Korea - [Register Now]
More Upcoming Global Events






Comments