Liposuction: 5 Fatal Complications and How To Prevent Them
- Jan 19, 2024
- 19 min read
Liposuction, a popular cosmetic surgery for body sculpting and fat removal, is generally considered safe; however, it is crucial to recognize that, like any surgical procedure, it carries a range of potential complications. These complications can be classified into mild, temporary issues and more severe problems, with rare instances leading to fatal outcomes. The overall complication rate is approximately 5%, with the majority being minor concerns. Nevertheless, studies have revealed a concerning statistic indicating that deaths associated with liposuction may occur in as many as 1 in every 5,000 surgeries.
On the less severe side, many patients may encounter temporary side effects such as swelling and bruising, which are deemed normal aspects of the healing process. Discomfort is also common but typically resolves with time and proper postoperative care. Despite being bothersome, these mild complications are generally manageable and do not pose significant risks to the overall health of the patient.
Advancing along the spectrum, more serious complications may emerge, including the potential risk of blood clot formation. Although this complication is relatively rare, its severity lies in the possibility of these clots traveling through the bloodstream and causing blockages in vital organs, thereby posing a life-threatening risk. This article will delve into the five most fatal complications of liposuction and provide insights on how to effectively prevent them.
I. Thromboembolic Disease
Thromboembolic disease is a medical condition characterized by the development of blood clots, or thrombi, which can traverse the circulatory system and result in blockages within blood vessels. This term encompasses two closely linked conditions: thrombosis, involving the creation of blood clots within blood vessels, and embolism, which occurs when these clots dislodge and travel to other parts of the body. Thromboembolic events carry significant consequences, as these clots can impede blood flow, causing damage to tissues, impairment of organ function, and, in severe instances, life-threatening complications like heart attacks or strokes.
Thromboembolic Disease in Liposuction
The potential for thromboembolic disease is a noteworthy concern in liposuction procedures, stemming from the complex interplay of various factors inherent in the surgical process. Liposuction, designed to eliminate excess fat through suction from specific body areas, can elicit physiological responses that foster the formation of blood clots. The disruption of fatty tissues and blood vessels during liposuction triggers the coagulation cascade, a sequence of events leading to blood clot development. The trauma induced by cannula insertion for fat aspiration initiates the release of pro-coagulant substances and promotes platelet aggregation, creating a conducive environment for clot formation.
Furthermore, the liposuction procedure often involves the infusion of tumescent fluid—a mixture of saline, local anesthetic (typically containing lidocaine), and epinephrine—into targeted areas. While this fluid aids in fat removal and minimizes bleeding, it introduces additional factors that contribute to thrombosis. Lidocaine's vasoconstrictive effects, for instance, may impact blood flow, and the overall increase in fluid volume can alter blood viscosity.
Factors in Thromboembolic Disease Factors
Thromboembolic disease results from a complex interplay of genetic, environmental, and health-related factors. Certain individuals possess an inherent inclination toward abnormal blood clotting, while specific situations or conditions can further amplify the risk. The following outlines key factors and groups more prone to thromboembolic events:
1. Inherited Genetic Factors: Some individuals inherit a disposition for abnormal blood clotting, exemplified by conditions like the Factor V Leiden mutation, prothrombin gene mutation, and other inherited thrombophilias, heightening the risk of clot formation.
2. Advancing Age: The likelihood of thromboembolic events generally escalates with age. Elderly individuals often experience slower blood flow, diminished vascular elasticity, and other factors contributing to clot formation.
3. Underlying Medical Conditions: Specific medical conditions predispose individuals to thromboembolism, including cancer, autoimmune disorders, cardiovascular diseases (such as atrial fibrillation), and inflammatory conditions.
4. Excess Body Weight: Increased susceptibility to thromboembolic disease is associated with obesity. Adipose tissue generates substances that induce inflammation and activate the clotting cascade.
5. Prolonged Immobility: Extended periods of immobility, such as during lengthy flights or post-surgical bed rest, can result in blood stasis, heightening the risk of clot formation.
6. Tobacco Use: Smoking stands as a significant risk factor for cardiovascular diseases and contributes to blood clot development. Nicotine and other components of tobacco smoke impact blood vessel function.
7. Pregnancy and Postpartum Period: Pregnant women face an elevated risk of thromboembolic events, particularly during the postpartum period. Hormonal shifts, increased blood volume, and compression of blood vessels by the expanding uterus contribute to this heightened risk.
8. Use of Hormonal Contraceptives: Birth control pills, especially those containing estrogen, can heighten the risk of clot formation, particularly in women with additional risk factors.
9. Surgical Interventions and Trauma: Major surgeries, including procedures like liposuction, can transiently increase the risk of blood clots. Trauma and injury can also contribute to clot formation.
10. Dehydration: Inadequate fluid intake can elevate blood viscosity, fostering clot formation.
Thromboembolic Disease Prevention
To mitigate the risk of thromboembolic disease in liposuction, surgeons implement preventive measures such as utilizing compression garments, encouraging early patient ambulation postoperatively, and, in some cases, administering prophylactic anticoagulant medications. Despite these measures, the occurrence of thromboembolic complications underscores the significance of meticulous patient selection, precise surgical techniques, and adherence to established safety protocols in the practice of liposuction.
Proactive measures and interventions for thromboembolic disease often involve anticoagulant medications, which hinder the formation of blood clots. These medications play a crucial role in both preventing and managing thromboembolic disease, including cases related to surgical procedures like liposuction. Their mechanism involves interference with the blood clotting process, thereby reducing clot formation and impeding their potential to cause vessel blockages.
Various anticoagulant medications exist, each with its unique mode of action. A common class is heparins, which can be administered intravenously or subcutaneously. Heparins enhance the activity of antithrombin, a natural anticoagulant in the body, resulting in the inhibition of several clotting factors. Another widely used anticoagulant type is warfarin, which disrupts the synthesis of clotting factors in the liver by inhibiting vitamin K. Typically taken orally, warfarin necessitates careful monitoring of the International Normalized Ratio (INR) to balance effectiveness and avoid excessive bleeding.
In the context of liposuction and other surgeries, prophylactic anticoagulants may be employed to diminish the risk of postoperative thromboembolic complications, particularly in patients with recognized risk factors such as a history of clotting disorders, obesity, immobility, or advanced age.
However, the use of anticoagulant medications demands a careful balance, as excessive anticoagulation can lead to bleeding complications. Healthcare providers assess individual patient risk factors to tailor the choice and dosage of anticoagulants accordingly. Postoperative management may involve the continuation of anticoagulants for a specified duration, transitioning gradually to additional preventive measures like compression garments and early ambulation.
II. Fat Embolism
Fat embolism is an uncommon yet potentially severe medical condition wherein fat particles infiltrate the bloodstream, traveling to distant organs and causing blockages in blood vessels. The primary cause of fat embolism is often the fracture of elongated bones, such as the femur or tibia, permitting fat from the bone marrow to enter the bloodstream. Additionally, fat embolism can manifest as a complication in various medical procedures, including orthopedic surgeries like hip or knee replacements, as well as traumatic injuries such as severe soft tissue injuries or burns.
As fat emboli traverse the bloodstream, they can become lodged in small blood vessels, particularly in crucial organs like the lungs and brain. The lungs are commonly affected, resulting in respiratory symptoms. The release of fat particles induces an inflammatory response, causing damage to blood vessel walls and potentially leading to respiratory distress. Symptoms of a fat embolism may encompass shortness of breath, rapid breathing, chest pain, confusion, and, in severe instances, unconsciousness.
The severity of fat embolism varies, ranging from mild cases that resolve spontaneously to severe cases that pose a life-threatening risk. Diagnosis typically involves clinical evaluation, imaging studies such as chest X-rays, and, in certain instances, blood tests to identify fat particles circulating in the bloodstream.
Fat Embolism in Liposuction
Fat embolism in the context of liposuction arises from the disturbance of adipose tissue during the surgical process, leading to the liberation of fat particles into the bloodstream. Liposuction entails the extraction of surplus fat deposits from specific body areas using a cannula—a slender tube—connected to a vacuum or suction device. The mechanical disruption of fatty tissue in this procedure can inadvertently introduce fat droplets into the circulatory system.
Once released into the bloodstream, these fat particles, referred to as emboli, can traverse blood vessels, potentially reaching distant organs and causing blockages. The primary target for fat embolism in liposuction is often the lungs, where emboli may lodge in small blood vessels, giving rise to respiratory complications. The intricate network of blood vessels in the lungs renders them particularly susceptible to fat embolism, manifesting symptoms such as shortness of breath, rapid breathing, chest pain, and, in severe cases, respiratory distress.
The mechanism of fat embolism in liposuction is intricately linked to the procedural nature. The application of negative pressure during suction, coupled with the mechanical disruption of adipose tissue, heightens the probability of fat particles entering the bloodstream. Additionally, factors such as the volume of fat removed, the speed of the procedure, and the surgical technique employed can influence the degree of fat embolism risks.
Factors in Fat Embolism
Fat embolism in liposuction is subject to various influencing factors, and specific individuals may exhibit a higher predisposition to this infrequent yet potentially severe complication. Grasping these factors is imperative for both surgeons and patients to effectively manage and reduce the associated risks.
1. Volume and Speed of Fat Removal: The quantity of fat removed and the velocity of aspiration during liposuction contribute to the risk of fat embolism. Swift and forceful removal of substantial fat volumes may escalate the likelihood of fat particles entering the bloodstream.
2. Surgeon's Technique: The surgical technique adopted significantly influences the risk of fat embolism. Delicate and controlled methods that prioritize fat preservation and minimize trauma to adjacent tissues are linked to a lower risk compared to more aggressive approaches.
3. Patient Health and Characteristics: Certain patient-related factors contribute to an increased vulnerability to fat embolism. Individuals with pre-existing medical conditions, such as cardiovascular diseases or clotting disorders, may face a higher risk. Moreover, patients with elevated body mass index (BMI) may have increased adipose tissue, potentially heightening the likelihood of fat embolism.
4. Procedural Considerations: Liposuction procedures encompassing multiple body areas or extended surgical durations may amplify the risk of fat embolism. The cumulative effect of prolonged procedures can increase trauma and the release of fat particles into the bloodstream.
5. Patient Positioning: The positioning of the patient during liposuction can influence the risk of fat embolism. Certain positions, especially those allowing for the pooling of fat in large vessels before suction, may heighten the chances of fat particles entering the bloodstream.
6. Pre-existing Health Conditions: Individuals with specific health conditions, such as compromised pulmonary function or vascular integrity, may exhibit greater susceptibility to the effects of fat embolism. Thorough preoperative assessments are vital for surgeons to evaluate the overall health status of patients before recommending or performing liposuction.
7. Surgeon's Experience and Expertise: The proficiency and expertise of the surgeon conducting liposuction are crucial factors. Skilled and knowledgeable surgeons are likely to employ techniques that minimize complications, including fat embolism. Rigorous preoperative assessments and adherence to safety protocols contribute to safer outcomes.
Fat Embolism Prevention
To minimize the risk of fat embolism in liposuction, a comprehensive approach involving preventive measures, careful surgical techniques, and prompt complication recognition is crucial. Surgeons can significantly decrease the likelihood of fat embolism by implementing the following strategies:
1. Thorough Preoperative Assessments: Identifying patients at higher risk for complications, such as those with cardiovascular diseases, clotting disorders, or respiratory issues, through thorough preoperative assessments is critical for risk minimization. Thoughtful patient selection plays a pivotal role in reducing risk.
2. Controlled Volume and Speed of Fat Removal: Adopting a conservative approach during surgery, limiting the amount of fat extracted in a single session, and controlling the speed of aspiration are crucial. Utilizing techniques that prioritize gentle tissue handling, such as smaller cannulas and controlled movements, minimizes trauma and reduces the risk of fat particles entering the bloodstream.
3. Utilizing Smaller Cannulas and Controlled Movements: The use of smaller cannulas during liposuction ensures precise and accurate fat removal, preserving the integrity of fat cells. Controlled movements play a crucial role in maintaining the structural integrity of adipose tissue, minimizing mechanical trauma to blood vessels and surrounding tissues.
4. Avoiding Excessive Force: Minimizing negative pressure during suctioning by avoiding excessive force and adopting smaller cannulas reduces the risk of fat embolism. Aggressive suctioning with larger cannulas and excessive force can create higher negative pressure, increasing the likelihood of drawing fat particles into the bloodstream.
5. Tumescent Fluid Composition: The inclusion of a vasoconstrictor, such as epinephrine, in the tumescent fluid helps minimize bleeding, reduce systemic absorption of local anesthetic, and create a controlled surgical field. This component contributes to a hemostatic effect, limiting the potential entry of fat particles into the bloodstream and enhancing overall safety during liposuction.
6. Continuous Postoperative Monitoring: Early recognition of complications is paramount, involving continuous monitoring of vital signs, respiratory function, and overall patient well-being postoperatively. Immediate attention is given to any deviation from the expected recovery.
7. Effective Complication Management: In case of fat embolism complications, supportive care is provided, including oxygen therapy to support respiratory function, intravenous fluids for hydration, and, in severe cases, mechanical ventilation. Corticosteroid therapy may be employed to reduce inflammation associated with fat embolism, and collaboration with multidisciplinary teams ensures a specialized approach to complication management.
8. Communication and Transparency: Clear communication with the patient and their family throughout the process is crucial. Keeping them informed about the complication, the steps being taken for management, and the expected course of recovery fosters trust and understanding.
9. Adaptation of Surgical Plan: In the event of complications, adjustments to the surgical plan, modifications to anesthesia, or temporary halting of the procedure may be considered to stabilize the patient and prevent further complications.
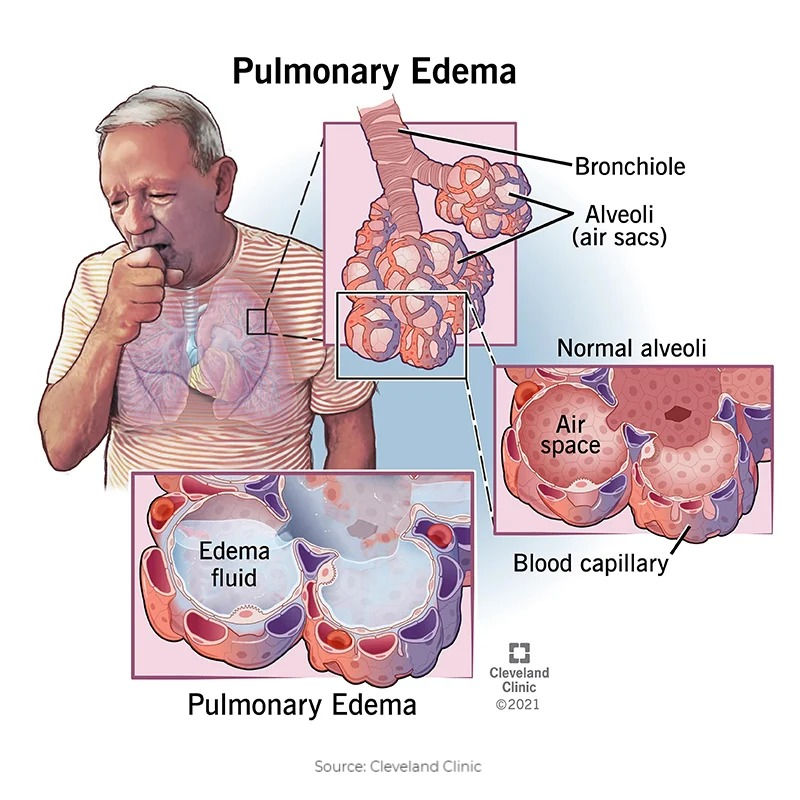
III. Pulmonary Edema
Pulmonary edema is a medical condition characterized by the abnormal accumulation of excess fluid in the lungs, particularly within the air sacs and surrounding lung tissues. This accumulation disrupts the normal exchange of oxygen and carbon dioxide, resulting in respiratory difficulties. The two main types of pulmonary edema are cardiogenic and non-cardiogenic:
1. Cardiogenic Pulmonary Edema:
This occurs when the heart struggles to pump blood effectively, leading to increased pressure within the pulmonary veins. Elevated pressure forces fluid into the lungs, impairing respiratory function. Common causes include heart failure, myocardial infarction (heart attack), or other cardiovascular conditions that strain the heart's pumping ability.
2. Non-Cardiogenic Pulmonary Edema:
This type often associated with injuries, infections, or acute respiratory distress syndrome (ARDS). Lung tissue becomes permeable, allowing fluid to leak into the air spaces. Triggers may include severe infections, inhalation of toxic substances, or traumatic injuries.
Symptoms of pulmonary edema encompass shortness of breath, wheezing, a persistent cough producing frothy or pink-tinged sputum, and a sensation of suffocation. Severe cases can progress to respiratory failure, necessitating immediate medical intervention. Diagnosis typically involves chest X-rays and other imaging studies to visualize the extent of fluid accumulation in the lungs
Pulmonary Edema in Liposuction
The occurrence of pulmonary edema in the context of liposuction is a rare but potentially severe complication. The underlying mechanism involves the inadvertent introduction of fat particles into the bloodstream during the liposuction procedure, particularly associated with large-volume liposuction where substantial amounts of adipose tissue are removed in a short timeframe. The sequence begins with the dislodgment of fat cells, forming fat emboli that can travel through the bloodstream, eventually reaching the pulmonary vasculature.
In the lungs, these fat emboli have the potential to obstruct small blood vessels, disrupting normal blood flow. This obstruction initiates an inflammatory response, increasing the permeability of lung capillaries. Consequently, fluid from the bloodstream leaks into the surrounding lung tissues and air sacs, leading to the development of pulmonary edema. The accumulation of fluid in the lungs impedes the efficient exchange of oxygen and carbon dioxide, resulting in respiratory distress.
Factors in Pulmonary Edema
Pulmonary edema is influenced by various factors, and certain individuals may be more susceptible to this condition. Cardiovascular health is a significant factor, with individuals having pre-existing heart conditions such as congestive heart failure or coronary artery disease being at an elevated risk. In these cases, compromised heart function may result in inadequate blood pumping, leading to fluid accumulation in the lungs.
High blood pressure is another contributing factor to pulmonary edema. Hypertension can strain lung blood vessels, increasing their vulnerability to leakage and fluid buildup. Conditions like acute respiratory distress syndrome (ARDS) and severe lung infections, including pneumonia, can induce non-cardiogenic pulmonary edema by enhancing the permeability of lung capillaries.
In the context of liposuction, as discussed earlier, the risk of pulmonary edema is linked to the volume and speed of fat removal. Procedures involving large volumes of fat and rapid extraction heighten the potential for fat embolism, which may subsequently lead to pulmonary edema. Patients with compromised cardiovascular health or underlying respiratory conditions may face a higher risk of severe complications during liposuction.
Additional risk factors include age, with older individuals generally having an increased risk of cardiovascular issues, and obesity, which can impose strain on the cardiovascular system. Smoking and a history of pulmonary problems may also contribute to an elevated susceptibility to pulmonary edema. Recognizing these risk factors is crucial for both healthcare providers and patients in assessing and managing potential complications associated with pulmonary edema.
Pulmonary Edema Prevention
Preventing pulmonary edema in the context of liposuction requires a comprehensive approach involving careful patient selection, precise surgical techniques, and diligent postoperative monitoring. Surgeons should conduct thorough preoperative assessments, with a particular focus on evaluating cardiovascular health, to identify individuals at a higher risk for complications, including pulmonary edema. Patients with pre-existing heart conditions, hypertension, or other cardiovascular issues may necessitate a more cautious approach.
During the liposuction procedure, prioritizing techniques that gently handle tissues is paramount. The use of smaller cannulas, controlled movements, and the avoidance of excessive force are crucial in minimizing trauma to blood vessels and adipose tissue, thereby reducing the risk of fat embolism—a primary contributor to pulmonary edema. Limiting the volume of fat removal in a single session and avoiding overly aggressive suctioning also play pivotal roles in preventing complications.
Postoperative monitoring is equally critical. Continuous observation of vital signs, respiratory function, and overall patient well-being enables the early detection of any signs of distress, facilitating prompt intervention if necessary. This vigilance is essential in mitigating the risk of severe complications, such as pulmonary edema.
In the event that pulmonary edema does occur, effective management involves providing supportive care and addressing the underlying cause. Oxygen therapy is administered to support respiratory function, and intravenous fluids may be given to maintain hydration. In severe cases, mechanical ventilation may be required to assist with breathing. Identifying and treating the root cause, whether it be cardiac issues, infection, or fat embolism, is crucial for effective management.
IV. Lidocaine Intoxication
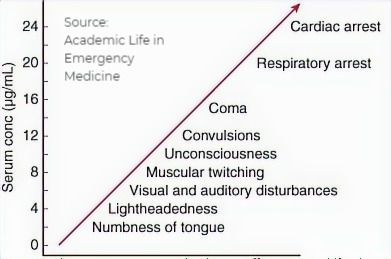
Lidocaine intoxication refers to an overdose or toxic reaction to lidocaine, a local anesthetic commonly used in various medical procedures, including liposuction. Lidocaine works by blocking nerve signals in the body, providing localized pain relief. However, when administered excessively or absorbed into the bloodstream beyond safe levels, lidocaine can lead to intoxication, resulting in adverse systemic effects.
Symptoms of lidocaine intoxication can range from mild to severe and may include dizziness, confusion, blurred vision, seizures, and, in extreme cases, cardiac arrest. The risk of lidocaine intoxication is heightened in procedures like liposuction, where large volumes of tumescent fluid containing lidocaine are injected into subcutaneous tissues to facilitate fat removal. The absorption of lidocaine into the systemic circulation can occur, especially when recommended dosage limits are exceeded.
Lidocaine intoxication is potentially life-threatening due to its impact on vital physiological systems, particularly the central nervous system (CNS) and the cardiovascular system. Lidocaine's mechanism of action involves blocking nerve signals, and when systemic levels become toxic, it can lead to profound effects on the body.
Cardiac effects are a primary concern in lidocaine intoxication, as the drug can disrupt the normal electrical rhythm of the heart, leading to ventricular arrhythmias or, in extreme cases, cardiac arrest. This impairs cardiac function, jeopardizing blood flow to critical organs and setting the stage for potentially fatal complications. Neurological manifestations include seizures, loss of consciousness, and respiratory arrest. Seizures are particularly dangerous, posing a risk of injury and complicating overall management. Lidocaine's suppression of respiratory drive can result in respiratory depression, compromising the exchange of oxygen and carbon dioxide and leading to respiratory failure.
Metabolic acidosis is another significant factor in the lethality of lidocaine intoxication. Excessive lidocaine levels can contribute to an imbalance in the body's acid-base equilibrium, leading to systemic dysfunction and organ failure. The cumulative impact of these effects makes lidocaine intoxication a critical medical emergency requiring immediate attention and intervention.
Lidocaine Intoxication in Liposuction
Lidocaine intoxication in liposuction can occur due to the administration of excessive amounts of tumescent fluid, which contains lidocaine, during the procedure. Tumescent fluid is used to facilitate fat removal by injecting a mixture of saline, lidocaine (local anesthetic), and epinephrine (vasoconstrictor) into the targeted areas. While this technique enhances patient comfort and minimizes bleeding, the potential for lidocaine intoxication arises when the recommended dosage limits are surpassed.
Large-volume liposuction, where significant amounts of fat are targeted for removal, often involves the infusion of substantial volumes of tumescent fluid. In some cases, the sheer volume required for extensive fat extraction may lead to elevated levels of lidocaine in the bloodstream, especially if the infiltration rates are too rapid. Additionally, variations in individual patient characteristics, such as weight, metabolism, and overall health, can influence how lidocaine is absorbed and processed.
The mechanism involves the systemic absorption of lidocaine, leading to higher circulating levels than the body can effectively metabolize. As lidocaine enters the bloodstream, it can exert its effects beyond the intended local anesthetic action, impacting the central nervous system, the cardiovascular system, and other vital organs. The potential for lidocaine toxicity is particularly pronounced when combined with the epinephrine component of tumescent fluid, as vasoconstriction can slow the elimination of lidocaine, prolonging its presence in the systemic circulation.
Factors in Lidocaine Intoxication
Lidocaine intoxication factors in liposuction are influenced by various elements related to the patient, the surgical procedure, and the properties of the anesthetic agents used. Understanding these factors is crucial in identifying individuals who may be more prone to lidocaine intoxication and implementing preventive measures.
Patient-specific factors include the patient's weight, overall health, and individual variations in drug metabolism. Heavier individuals may require larger volumes of tumescent fluid for effective anesthesia, but this can increase the risk of lidocaine toxicity. Patients with compromised liver function may experience slower lidocaine metabolism, affecting the clearance of the drug from the body and elevating the risk of intoxication.
The volume and rate of tumescent fluid administration during liposuction play a significant role in lidocaine intoxication. Large-volume liposuction, where extensive fat removal is targeted, inherently involves higher amounts of tumescent fluid. Rapid infiltration rates, especially when combined with large volumes, can lead to a rapid rise in systemic lidocaine levels, increasing the likelihood of toxicity. Surgeons must carefully calibrate the dosage to the patient's characteristics and the extent of the liposuction procedure. Certain patient conditions may also predispose individuals to lidocaine intoxication.
Patients with pre-existing cardiovascular issues, such as arrhythmias or heart failure, are more vulnerable to the cardiac effects of lidocaine. Additionally, individuals with impaired kidney function may be at greater risk due to the potential accumulation of lidocaine metabolites. Moreover, the presence of epinephrine in the tumescent fluid, while aiding in vasoconstriction and minimizing bleeding, can contribute to the risk of lidocaine intoxication. The vasoconstrictive effects of epinephrine may slow down the clearance of lidocaine, leading to prolonged exposure and heightened toxicity levels. Individuals undergoing extensive liposuction, particularly those with multiple or large areas targeted for fat removal, are prone to lidocaine intoxication.
Lidocaine Intoxication Prevention
Preventing lidocaine intoxication in liposuction is crucial for ensuring the safety of the procedure. Several key measures can be implemented to minimize the risk of lidocaine toxicity. A comprehensive preoperative assessment is fundamental in identifying patients at higher risk for lidocaine intoxication. Factors such as the patient's weight, overall health, and pre-existing medical conditions, particularly those affecting liver function, should be carefully evaluated. This assessment guides the surgeon in determining the appropriate dosage and ensures that the patient is a suitable candidate for liposuction.
Surgeons must strictly adhere to recommended dosage guidelines for lidocaine. These guidelines take into account both the total volume of tumescent fluid and the maximum dosage of lidocaine per unit of body weight. Careful calculation based on these parameters helps prevent the administration of excessive amounts of lidocaine. The rate at which tumescent fluid, containing lidocaine, is infiltrated is a critical factor in preventing lidocaine intoxication. Slower infiltration rates reduce the risk of rapid systemic absorption and toxicity. Surgeons should monitor these rates closely throughout the procedure, adjusting them as needed to maintain patient safety.
Recognizing the uniqueness of each patient is essential in preventing lidocaine intoxication. An individualized approach to liposuction considers factors such as the extent of the procedure, the patient's overall health, and the presence of coexisting conditions. This tailored approach ensures that the dosage and infiltration rates are adjusted based on individual characteristics, minimizing the risk of complications.
Vigilant intraoperative monitoring is critical for early detection of signs and symptoms of lidocaine intoxication. Regular assessments of the patient's vital signs, including heart rate, blood pressure, and oxygen saturation, help identify any deviations from the expected parameters. Early recognition enables prompt intervention and reduces the likelihood of severe complications.
Selection of anesthetic agents and the concentration of these agents should be carefully considered to optimize anesthesia while minimizing potential complications. Epinephrine, for example, can contribute to vasoconstriction, aiding in the control of bleeding and reducing systemic absorption of lidocaine.
In severe cases of lidocaine intoxication where cardiac arrhythmias or arrest occur, initiation of advanced cardiac life support (ACLS) protocols may be necessary. ACLS involves interventions such as defibrillation, administration of antiarrhythmic medications, and other measures to restore and maintain cardiac function. Immediate access to ACLS interventions is critical in managing life-threatening complications.
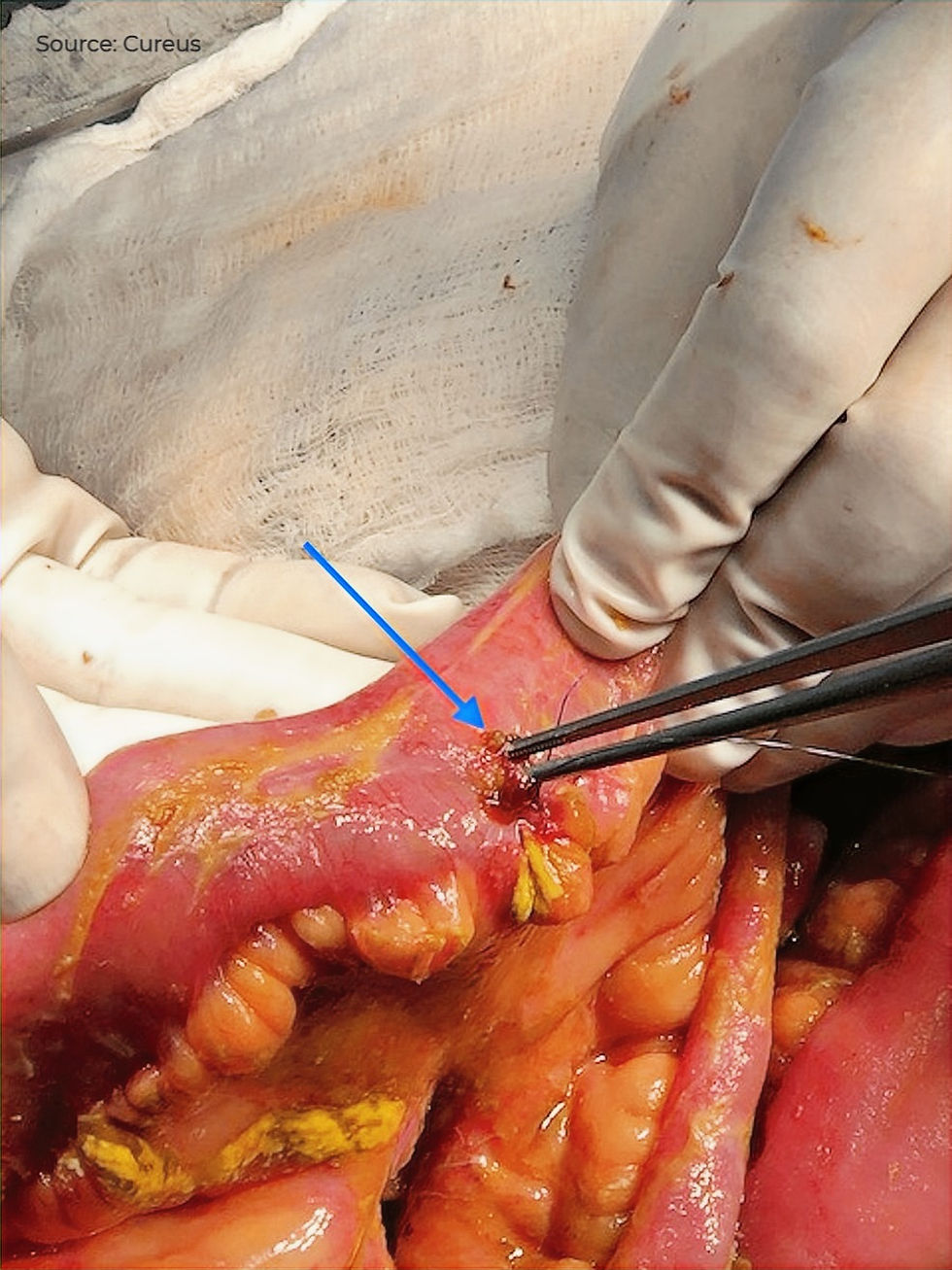
IIV. Intraabdominal Visceral Lesion
An intraabdominal visceral lesion refers to an abnormality or injury affecting the internal organs within the abdominal cavity. The abdominal viscera include essential organs such as the liver, spleen, stomach, intestines, and kidneys. An intraabdominal visceral lesion can encompass various conditions, ranging from structural abnormalities and tumors to traumatic injuries.
Intraabdominal visceral lesions may involve structural abnormalities within organs or the development of tumors. These abnormalities can be congenital, such as malformations or cysts, or acquired, resulting from conditions like inflammatory processes or neoplastic growths. Tumors arising within the abdominal viscera can be benign or malignant, and their presence may lead to a range of symptoms depending on their size, location, and impact on surrounding structures.
Traumatic injuries to the intraabdominal viscera can occur due to external forces, such as blunt or penetrating trauma. These injuries may result from accidents, falls, or intentional injuries. Common examples include liver or spleen lacerations, bowel perforations, or kidney injuries. Traumatic intraabdominal visceral lesions often require prompt medical attention and intervention to prevent complications like internal bleeding or infection.
The symptoms of intraabdominal visceral lesions can vary widely based on the specific organ affected and the nature of the lesion. Common symptoms may include abdominal pain, bloating, changes in bowel habits, weight loss, and, in some cases, visible masses or swelling. Diagnostic approaches often involve imaging studies such as CT scans, MRI, or ultrasound to visualize the affected organs and identify the nature and extent of the lesion. In some cases, more invasive procedures like exploratory surgery or endoscopy may be necessary for a definitive diagnosis.
Intraabdominal Visceral Lesions in Liposuction
In the context of liposuction, intraabdominal visceral lesions can potentially occur as a result of the surgical procedure's impact on the abdominal area. Liposuction involves the removal of excess fat from specific regions of the body, and when performed on the abdominal region, there is a risk of inadvertently affecting the underlying visceral organs.
During liposuction, a surgeon typically inserts a thin tube called a cannula through small incisions in the skin to suction out excess fat. However, if the cannula is not properly guided or if excessive force is applied during the procedure, it may puncture or damage the protective layers surrounding intraabdominal organs. This unintended trauma can lead to lesions on the visceral organs such as the liver, spleen, or intestines.
The abdominal cavity contains vital organs with delicate structures, and any disruption or injury to these structures can result in intraabdominal visceral lesions.
Factors and Prevention in Intraabdominal Visceral Lesions
The severity of the lesions can vary based on factors such as the surgeon's skill, the patient's anatomy, and the overall technique employed during liposuction. Preventing intraabdominal visceral lesions in liposuction requires meticulous surgical technique, proper cannula placement, and careful adherence to safety guidelines. Surgeons must be attentive to the depth and force applied during the procedure to minimize the risk of unintended damage to underlying organs. Additionally, thorough preoperative assessments help identify any anatomical variations or pre-existing conditions that may increase the susceptibility to such injuries.
In conclusion, while liposuction remains a sought-after cosmetic solution for body contouring and fat elimination, it is imperative to navigate the nuanced landscape of potential complications associated with the procedure. Despite being generally regarded as safe, liposuction, like any surgical intervention, introduces a spectrum of risks, ranging from mild and transient issues to rare but severe and, in some instances, fatal outcomes. Safeguarding against these potentially fatal complications necessitates a refined surgical approach, precise cannula placement, and unwavering commitment to safety guidelines. Surgeons must exercise caution in controlling the depth and force applied during the procedure to minimize the risk of unintended damage to underlying organs. Comprehensive preoperative assessments play a pivotal role in identifying anatomical variations or pre-existing conditions that might heighten susceptibility to injuries.
Reference:
Strategies for Reducing Fatal Complications in Liposuction (2017)
The safety of liposuction: results of a national survey (2002)
Analysis of postoperative complications for superficial liposuction: a review of 2398 cases (2011)
Major and lethal complications of liposuction: a review of 72 cases in Germany between 1998 and 2002 (2008)
Fatal outcomes from liposuction: census survey of cosmetic surgeons (2000)
Learn step-by-step techniques behind Liposuction & Fat Transfer
in our upcoming Mini Fellowship:
IFAAS Mini Visiting Fellowship (Hands-on)
Liposuction & Facial Fat Transfer Under Local Anaesthesia
Mar 20-21, 2024 - Seoul, South Korea - [Register Now]
More Upcoming Global Events










Comments